Revolutionizing Infection Treatment: The Role of Bacteriophages
Written on
Introduction to Bacteriophages
In light of recent global health crises, the general view of viruses is predominantly negative. Eukaryotic viruses, which can inflict diseases on humans, understandably evoke fear, given the substantial loss of life attributed to various viral infections annually. However, there exists another group of viruses that do not harm humans and may serve as a protective “immune system” against pathogenic bacteria. These beneficial viruses are known as bacteriophages, or phages for short. The term bacteriophage is derived from Latin, meaning "bacteria eater." Remarkably, phages are responsible for the elimination of over 20% of oceanic bacteria daily, underscoring their ecological significance. Some phages have been identified that effectively target bacteria responsible for serious illnesses such as staph infections, pneumonia, and tuberculosis. Despite their potential, phages have seldom been utilized in Western medicine due to historical developments surrounding the emergence of antibiotics.
The Historical Context: The Fight Against Infections
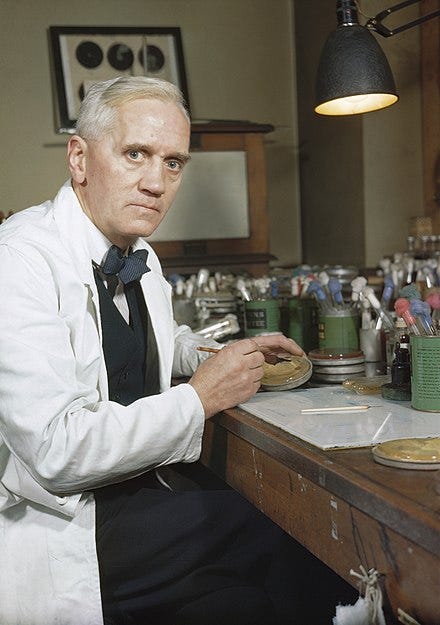
The early 20th century marked a significant period during World War I, where industrial warfare led to unprecedented injuries and subsequent infections among soldiers. The dire situation prompted researchers to seek effective solutions to combat deadly bacterial infections. In 1917, Felix d’Herelle, a French-Canadian scientist, discovered a previously unknown microbe capable of targeting the bacterium responsible for dysentery, which he named bacteriophages. Through collaboration with Russian researchers, d’Herelle applied phage therapy to treat bacterial infections during the 1920s and 1930s. However, the rise of antibiotics, particularly after Alexander Fleming’s groundbreaking discovery of penicillin, overshadowed phage therapies due to their broad-spectrum efficacy and ease of production.
The Challenge of Antibiotic Resistance
Antibiotic resistance, the phenomenon whereby bacteria evolve to resist the effects of medications designed to kill them, is a pressing global health issue. In the U.S. alone, there are approximately 2.8 million infections each year attributed to antibiotic-resistant bacteria, resulting in about 35,000 deaths annually, according to the CDC. The prevalence of such infections is anticipated to rise, necessitating innovative approaches to treatment. Companies like Endolytix, Felix, and Adaptive Phage Therapeutics are pioneering efforts to address antibiotic resistance, with phage therapy forming the foundation of their strategies.
The Consequences of Antibiotic Use
While antibiotics are critical for treating infections, research highlights their detrimental effects on the microbiome, disrupting the balance of beneficial bacteria. Antibiotics act indiscriminately, akin to deploying a nuclear weapon against bacteria, eradicating both harmful and beneficial strains. This loss of good bacteria can lead to an increase in antibiotic-resistant strains, which require even more potent antibiotics, further exacerbating the issue.

The Promise of Phage Therapy
Recently, the application of phage therapy has gained renewed interest in Western medicine, with 19 clinical trials currently underway at esteemed institutions like the Mayo Clinic, National Jewish Health, and Yale University. Numerous past studies demonstrate that phage therapy is both safe and effective in treating bacterial infections. Phages offer a targeted approach to combat antibiotic-resistant bacteria due to their specific host ranges, effectively acting as precision tools against harmful strains while preserving the beneficial bacteria in the microbiome.

Integrating Phages and Antibiotics
As phage therapy continues to evolve, it is becoming clear that phages can complement traditional antibiotic treatments. This collaboration represents a shift from the historical competition between these two treatment modalities during World War I to a more integrated approach. Phages are poised to transform conventional medical practices, paving the way for more personalized treatment strategies that incorporate both broad-spectrum antibiotics and targeted phage therapies. The prospect of using viruses to aid in disease treatment may seem unconventional, but it highlights the potential for innovative solutions in the face of rising antibiotic resistance.
Antimicrobial Resistance: Antibiotics do not treat viral infections like cold or flu - YouTube
This video explores the critical distinction between bacterial and viral infections, emphasizing the ineffectiveness of antibiotics against viral diseases.
Bacterial vs. Viral Infections: When is it Time for Antibiotics? - YouTube
The video discusses the importance of understanding the differences between bacterial and viral infections and when antibiotic intervention is necessary.
Conclusion
Bacteriophages are emerging as a pivotal player in the battle against antibiotic-resistant infections. With ongoing research and clinical trials, the potential for phage therapy to revolutionize infection treatment is becoming increasingly evident. As we continue to explore these innovative solutions, the role of viruses in medicine may soon shift from a source of fear to a beacon of hope.
About the Author
My name is Cody Glickman, and I can be found on LinkedIn. My graduate research focused on identifying phages within metagenomic datasets, likened to finding a viral needle in a DNA haystack. Explore some of my other works below:
Viruses inside Bacteria
Investigating the beneficial genes that enable bacteria to thrive.
Pfam Database Filtering Using Python
Techniques for selecting Hidden Markov Models (HMM) through string searching.
Google’s Project Nightingale and Emergent Medical Data
Insights into how health data can reveal information about individuals.