Innovative Approaches to Cancer Vaccination: A Comprehensive Look
Written on
Chapter 1: The Quest for a Cancer Vaccine
Imagine a world where we could shield ourselves from cancer! While it may seem like a distant dream, advancements in medical science are paving the way for potential breakthroughs. Cancer remains a formidable adversary, claiming the lives of nearly 599,000 individuals in the United States each year, making it the second leading cause of death after heart disease. This illness arises when our own cells begin to proliferate uncontrollably, driven by a series of mutations that alter their normal functions.
In many instances, cancer appears as a consequence of surviving other health challenges. Our cells are not immortal, and the mutations that lead to cancer accumulate over time. So, is it possible to create a vaccine that could protect us from this disease?
The answer lies in a specific subset of cancers linked to certain viruses. By vaccinating against these viruses, we could significantly lower the incidence of various cancers, including:
- Cervical cancer
- Oropharyngeal cancers (affecting the tongue and throat)
- Anal cancer
- Penile cancer
- Vaginal cancer
- Vulvar cancer
In the United States, approximately 45,000 cases of these cancers are diagnosed annually, with a particular virus responsible for around 36,000 of these cases.
The virus in question is the human papillomavirus (HPV). The Gardasil 9 vaccine is highly recommended to combat HPV, although it is not universally mandated across states.
Let's delve into how this virus can lead to cancer and reflect on the public discourse surrounding HPV vaccination that emerged about a decade ago.
Section 1.1: Understanding the Mechanism of Cancer Induction
HPV is not a singular virus but a collection of around 200 different strains, primarily transmitted through sexual contact. These viruses can affect various body parts, including the genitals, mouth, throat, and anus. Most strains are asymptomatic, while some can lead to warts, and a few can trigger cancer.
Like many viruses, HPV infiltrates host cells and commandeers their machinery to replicate itself. High-risk variants of HPV alter several cellular functions. One critical protein impacted is p53, known as the "guardian of the cell," which plays a crucial role in tumor suppression. This protein detects DNA damage and either repairs it or halts cell division to prevent cancerous growth.
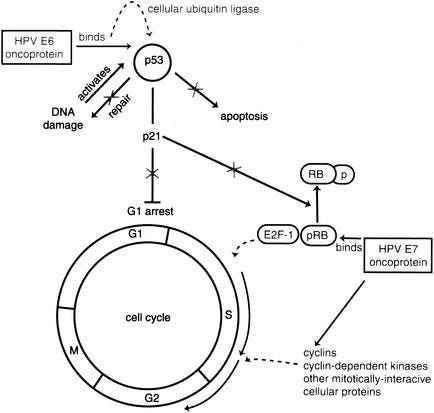
The high-risk HPV strains can deactivate p53, allowing the virus to replicate unchecked while simultaneously jeopardizing the cell's protective mechanisms. Without p53, cells are free to divide uncontrollably, increasing the risk of cancer.
Section 1.2: Vaccination: Our Best Defense Against HPV
To combat this family of viruses and the associated cancer risks, the most effective strategy is vaccination. Three vaccines are available to protect against the majority of HPV types: Gardasil, Gardasil 9, and Cervarix. In the U.S., Gardasil 9 is the standard, while the others are utilized in various countries.
These vaccines educate our immune system to identify HPV particles, prompting the production of antibodies that target and neutralize the virus. Importantly, these vaccines do not contain live virus; instead, they feature virus-like particles that mimic the virus's outer shell, devoid of its DNA. This approach is akin to having a computer casing without the internal components—recognizable, yet inactive.
These particles effectively stimulate the immune system, training it to produce the necessary antibodies that would also target the actual virus.
Chapter 2: A Tale of Two Regions: HPV Vaccination Outcomes
The first video titled "What's the next frontier for cancer vaccine development and research?" discusses emerging trends and potential future directions in cancer vaccine research.
In 2007, a public health experiment unfolded in two contrasting regions: Texas and Australia. In Texas, a proposed HPV vaccine mandate faced rejection, resulting in low vaccination rates (48% in 2019). Conversely, Australia offered the HPV vaccine for free to adolescent girls, achieving an impressive 80% vaccination rate.
The outcome? Australia is on track to potentially eradicate cervical cancer within the next decade, while Texas grapples with one of the highest cervical cancer rates in the nation, comparable to some developing countries.
The Texas Tribune provided an in-depth analysis of the state's struggle to adopt the HPV vaccine, highlighting how political resistance hindered public health initiatives.
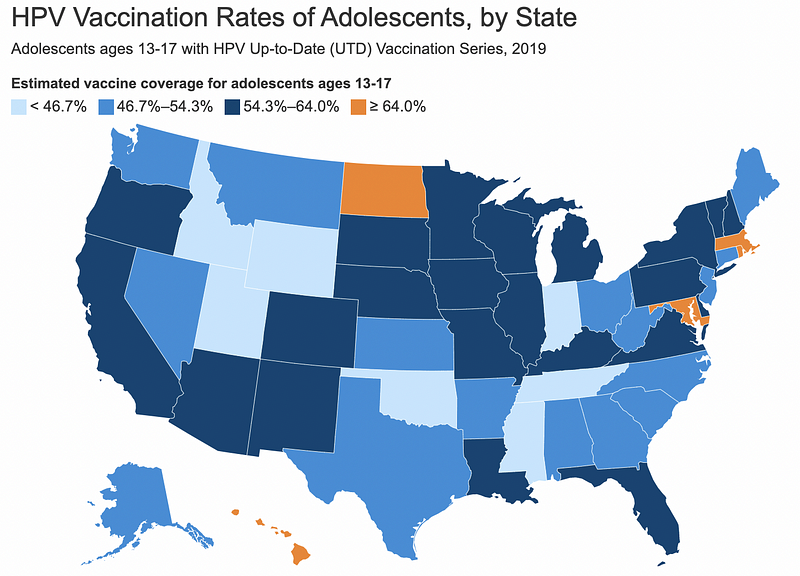
Across the United States, vaccination rates for HPV vary significantly, with the lowest percentages often found in southeastern states where political resistance is prevalent.
Summary: The Role of Vaccination in Cancer Prevention
While we cannot receive a vaccine directly against cancer, we can protect ourselves against HPV, the virus responsible for most cervical cancer cases. HPV infections can disable our cells' natural defenses against cancer, increasing susceptibility to the disease. Vaccination against HPV helps mitigate this risk, offering a protective measure against cancer.
Unfortunately, the anti-vaccine sentiment continues to pose challenges in safeguarding our youth from HPV, leaving them more vulnerable to cancer. It's a perplexing stance, as who would genuinely advocate for an increased cancer risk?
For those without the HPV vaccine, it's still available through primary care providers for both men and women up to age 45. It's a remarkable achievement of modern medicine—an opportunity to protect ourselves through vaccination!